Shaping the Future of Therapeutics
Poster Session B
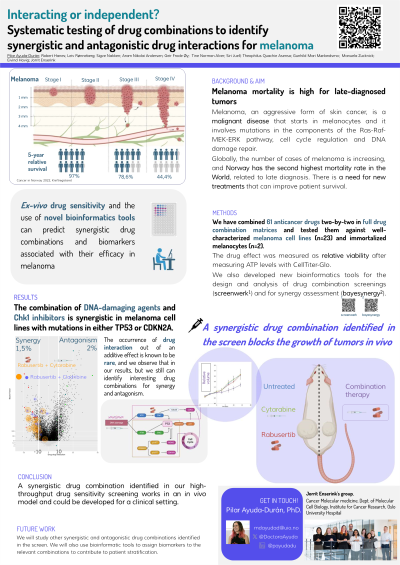
(1057-B) Interacting or independent? Systematic testing of drug combinations to identify synergistic and antagonistic drug interactions for melanoma
Wednesday, May 29, 2024
10:30 - 11:15 CEST
Location: Exhibit Hall

Pilar Ayuda-Durán (she/her/hers)
Head engineer/Lab manager/researcher
Oslo University Hospital
Oslo, Oslo, Norway
Poster Presenter(s)
Abstract: Melanoma, an aggressive form of skin cancer, is a malignant disease that starts in melanocytes and involves mutations in the Ras-Raf-MEK-ERK pathway, cell cycle regulation, and DNA damage repair pathway. Globally, the number of cases of melanoma is increasing, and mortality is high for late-diagnosed tumors despite the recent advances in melanoma treatment. There is a need for new treatments that can improve patient survival.
The development of treatment resistance is common and almost universal for targeted therapies and is caused because cancer therapies apply a strong selection pressure for resistance, leading to treatment failure and tumor progression. One strategy to overcome some of the treatment resistance mechanisms is to use drug combinations, especially if they show synergistic interactions.
Identifying such combinations is a difficult task. Traditionally, the creation of combination treatment courses has been an empirical exercise based on molecular and clinical knowledge. There is a great effort to find new and clinically relevant synergistic drug combinations, but the occurrence of synergy is rare, and the effects observed in the clinic, even for well-established combination courses, are mainly due to additive effect. In this scenario, the establishment of a standardized design and analysis method for finding synergistic drug combinations has great potential to improve cancer treatment.
In our project, we have combined 61 anticancer drugs two-by-two in full drug combination matrices and tested them against melanoma cell lines (n=23) and immortalized melanocytes (n=2) using a high-throughput ex-vivo drug sensitivity screen. The drug effect was measured as relative viability after measuring ATP levels with CellTiter-Glo. Thanks to our optimization efforts we have developed a very reliable and reproducible protocol, published in 2023. We also developed new bioinformatics tools to design and analyze drug combination screenings (screenwerk) and synergy assessments (bayesynergy), getting a classification of synergistic, antagonistic, or non-interactive for each drug pair in each cell line.
Our results confirm that synergy and antagonism are rare while non-interactive effects are more common. Although rare, we have identified some interesting drug combinations in melanoma cell lines. One example that we have further validated is the high synergy observed in the combination of DNA-damaging agents and Chk1 inhibitors on cells that have a compromised DNA damage response due to mutations in TP53 and CDKN2A. Experiments in mice xenografted with one of the sensitive melanoma-derived cell lines confirm that this combination is efficient also in vivo, while showing no toxicity for the mice.
In conclusion, we have generated a high-quality drug combination dataset on melanoma, identifying a synergistic drug combination that works in an in vivo model and could be developed further as a melanoma treatment. Our system can be expanded to other tumor types, improving patient stratification and cancer therapy.
The development of treatment resistance is common and almost universal for targeted therapies and is caused because cancer therapies apply a strong selection pressure for resistance, leading to treatment failure and tumor progression. One strategy to overcome some of the treatment resistance mechanisms is to use drug combinations, especially if they show synergistic interactions.
Identifying such combinations is a difficult task. Traditionally, the creation of combination treatment courses has been an empirical exercise based on molecular and clinical knowledge. There is a great effort to find new and clinically relevant synergistic drug combinations, but the occurrence of synergy is rare, and the effects observed in the clinic, even for well-established combination courses, are mainly due to additive effect. In this scenario, the establishment of a standardized design and analysis method for finding synergistic drug combinations has great potential to improve cancer treatment.
In our project, we have combined 61 anticancer drugs two-by-two in full drug combination matrices and tested them against melanoma cell lines (n=23) and immortalized melanocytes (n=2) using a high-throughput ex-vivo drug sensitivity screen. The drug effect was measured as relative viability after measuring ATP levels with CellTiter-Glo. Thanks to our optimization efforts we have developed a very reliable and reproducible protocol, published in 2023. We also developed new bioinformatics tools to design and analyze drug combination screenings (screenwerk) and synergy assessments (bayesynergy), getting a classification of synergistic, antagonistic, or non-interactive for each drug pair in each cell line.
Our results confirm that synergy and antagonism are rare while non-interactive effects are more common. Although rare, we have identified some interesting drug combinations in melanoma cell lines. One example that we have further validated is the high synergy observed in the combination of DNA-damaging agents and Chk1 inhibitors on cells that have a compromised DNA damage response due to mutations in TP53 and CDKN2A. Experiments in mice xenografted with one of the sensitive melanoma-derived cell lines confirm that this combination is efficient also in vivo, while showing no toxicity for the mice.
In conclusion, we have generated a high-quality drug combination dataset on melanoma, identifying a synergistic drug combination that works in an in vivo model and could be developed further as a melanoma treatment. Our system can be expanded to other tumor types, improving patient stratification and cancer therapy.
