Frontiers in Technology
Poster Session B
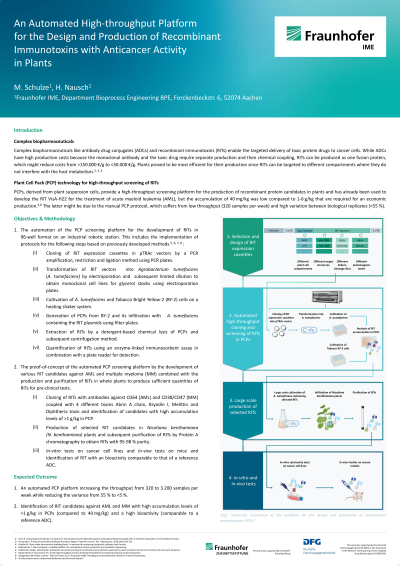
(1029-B) Development of an Automated High-throughput Platform for the Design and Production of Recombinant Immunotoxins with Anticancer Activity in Plant Cells
Wednesday, May 29, 2024
10:30 - 11:15 CEST
Location: Exhibit Hall
.jpg)
Monique Schulze (she/her/hers)
PhD
Fraunhofer Institute for Molecular Biology and Applied Ecology IME
Aachen, Nordrhein-Westfalen, Germany
Poster Presenter(s)
Abstract: Complex biopharmaceuticals, such as antibody drug conjugates (ADCs) and recombinant immunotoxins (RITs), enable targeted delivery of toxic protein drugs to cancer cells, increasing its efficiency while minimizing off-target effects compared to conventional chemotherapies. While ADCs consists of a monoclonal antibody fused to a synthetic small-molecule drug and need to be produced separately, which leads to production costs of 150,000 USD/g for common and 1,000,000 USD/g for rare cancer types, RITs consist of a mAb fused to a proteinogenic drug and can be produced as one fusion protein, reducing the costs below 30,000 USD/g. However, the RITs interfere with the host metabolism in mammalian cell lines and thus are produced at low accumulation levels of less than 10 mg/L, plants proofed to be suitable for their production, since they can express the RIT in the vacuole, where it does not impact the metabolism, yielding up to 300 mg/kg of the RIT. In addition, plants can be transiently transformed and thus produce relevant quantities within 1-3 months, while stably transformed cell lines require 6-12 months. In the transient transformation, wild-type plants are infected with a transgenic Agrobacterium tumefaciens (A. tumefaciens), carrying the expression vector, and the infected plants express and accumulate the target protein within 3-5 days without the need of stable integration into the chromosome. Since the production of biopharmaceuticals in whole plants proofed to be hardly compatible with the Good Manufacturing Practice (GMP) legislation, which is tailored to mammalian cells, the transient transformation has been transformed to Nicotiana tabacum plant cells via the patented Plant Cell Pack (PCP) technology, in which the suspension cells are packed to compact masses (cookies) which can be efficiently infected by the expression vector-containing A. tumefaciens. The PCP technology has already been used to develop the RIT VisA-H22 for the treatment of Acute Myeloid Leukemia (AML), but the accumulation of 40 mg/kg was comparably low. One reason for that might be the limited throughput of the PCP technology. Whereas the preparation of PCPs and its infection with the transgenic A. tumefaciens has already been optimized, manual handling is required for the cloning of the synthetic expression cassettes and vector, its subsequent transformation into A. tumefaciens, the cultivation of the transgenic A. tumefaciens as well as the cultivation of N. tabacum wild-type cells, so that only a few VisA-H22 variants could be screened. Another reason might be that the PCP technology suffers from large variation between biological replicates since the process has not been standardized, which impeded the screening and comparison of the tested Vis-H22 variants. Hence, these two bottlenecks will be addressed by automating the PCP technology using a robotic station and the automated PCP protocol to develop new anti-AML RITs with higher accumulation levels.
